Diabetic Retinopathy
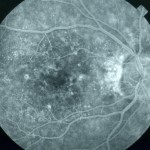
 Diabetic retinopathy is a complication of diabetes. The length of time a patient has diabetes will determine the likelihood of developing diabetic retinopathy. Over 40 percent of patients in the United States, diagnosed with diabetes, have a form of diabetic retinopathy. Diabetic retinopathy is the most common diabetic eye complication and the leading cause of blindness in American adults ages 25-65.
Diabetic retinopathy is a complication of diabetes. The length of time a patient has diabetes will determine the likelihood of developing diabetic retinopathy. Over 40 percent of patients in the United States, diagnosed with diabetes, have a form of diabetic retinopathy. Diabetic retinopathy is the most common diabetic eye complication and the leading cause of blindness in American adults ages 25-65.
Diabetic retinopathy causes the blood vessels that supply nourishment to the retina, the light-sensitive lining in the back of the eye where vision is focused, to weaken. These weakened vessels can leak, swell, or develop thin branches leading to bleeding in the eye; all causing a loss of vision. During any stage of diabetic retinopathy a condition known as macular edema can develop. Macular edema is the buildup of fluid in the macula, the light-sensitive part of the retina that allows us to see objects with great detail. As the macula swells vision becomes blurred. About half of the people with proliferative retinopathy are diagnosed with macular edema.
Treatment of Diabetic Retinopathy
Controlling blood pressure, blood cholesterol, and the levels of blood sugar is most important. Proliferative retinopathy is treated with a laser surgery procedure known as scatter laser treatment. During the procedure the abnormal blood vessels are ablated causing them to shrink. This procedure works best once the blood vessels begin to bleed. Severe blood vessel bleeding may need to surgically corrected with a vitrectomy procedure to remove the blood from the eye. Nonproliferative retinopathy with macular edema is treated usually with combination of intravitreal injections and a laser procedure called focal laser treatment. Intravitreal injections and focal laser treatment is performed in your doctor's office. The treatments help reduce the risk of vision loss and may improve lost vision in a small number of cases.
Retinal Detachment
Causes of a Retinal Detachment
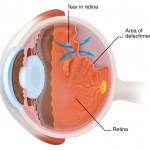
Retinal detachment can be complication of cataract surgery. A severe inflammation may alter the position of the retinal tissue and begin the detachment process. Other causes of a retinal detachment may be as follows:
- Nearsightedness
- A retinal tear
- Family history of retinal detachment
- Glaucoma
- Cataract surgery
- Trauma
- Existing eye condition
Symptoms of a Retinal Detachment
Symptoms of retinal detachment may progress slowly or rapidly, but both should be reported to a medical doctor as soon as possible so as to minimize the risk of vision loss. Some of the symptoms of a retinal detachment include:
- A sudden decrease in visual acuity
- A sudden increase in the amount of "floaters" in vision
- Bright flashes in the periphery
- An unnatural "curving" of straight lines
- Loss of central vision
- A dense shadow throughout the visual field
The patient should be taken to an emergency room as quickly as possible.
Treatment of a Retinal Detachment
To prevent permanent vision loss, the retina must be quickly reattached. Treatment for retinal detachment can be done through one or more of the following methods:
- Cryotherapy
- Laser photocoagulation
- Pneumatic retinopexy
- Scleral buckle
- Vitrectomy
Most surgeries to repair a retinal detachment are successful. In some cases, a second procedure will need to be performed. After a successful procedure, vision will take time to improve but may not return to previous levels of acuity.
Age-Related Macular Degeneration
The speed at which AMD advances is variable. In some patients, the condition progresses slowly and the changes in vision are imperceptible for some time. In others, the disease moves at an accelerated pace, leading relatively quickly to loss of central vision in one or both eyes. While AMD does not result in complete blindness because some peripheral vision always remains, it does make ordinary activities, particularly those that require close visual acuity, increasingly difficult.
Treatment of AMD
While there is not yet a cure for AMD, many patients have been helped greatly by recent innovations in treatment. Regular eye examinations to facilitate early detection of AMD are essential, since most therapies work best when started at an early stage of either type of the disorder. Even though treatments cannot reverse the disease process, they are often able to stop the progression of symptoms so the patient can maintain as much vision as possible.
Recommended treatments for AMD may include one or more of the following, each of which approaches controlling AMD in a somewhat different way:
- Vitamin and mineral supplementation known as AREDS
- Injections of anti-VEGF (vascular endothelial growth factor)
- Laser therapy
- Laser submacular surgery
- Use of low vision aids
An innovative device, known as an implantable miniature telescope (IMT) has been designed to be implanted in place of the patient's natural lens. While not a cure for AMD, it offers hope for much improved vision for those with the disorder.